Eosinophilic Esophagitis: An Emerging Allergic Disease
Eosinophilic esophagitis (EoE) is a chronic immune/antigen-mediated esophageal disease characterized clinically by symptoms related to esophageal dysfunction and histologically by eosinophil-predominant inflammation. Over the past 20 years, EoE has emerged as a major cause of dysphagia and food impaction. In this article, we discuss the pathogenesis, clinical presentation, diagnosis and management of this allergy-related condition.
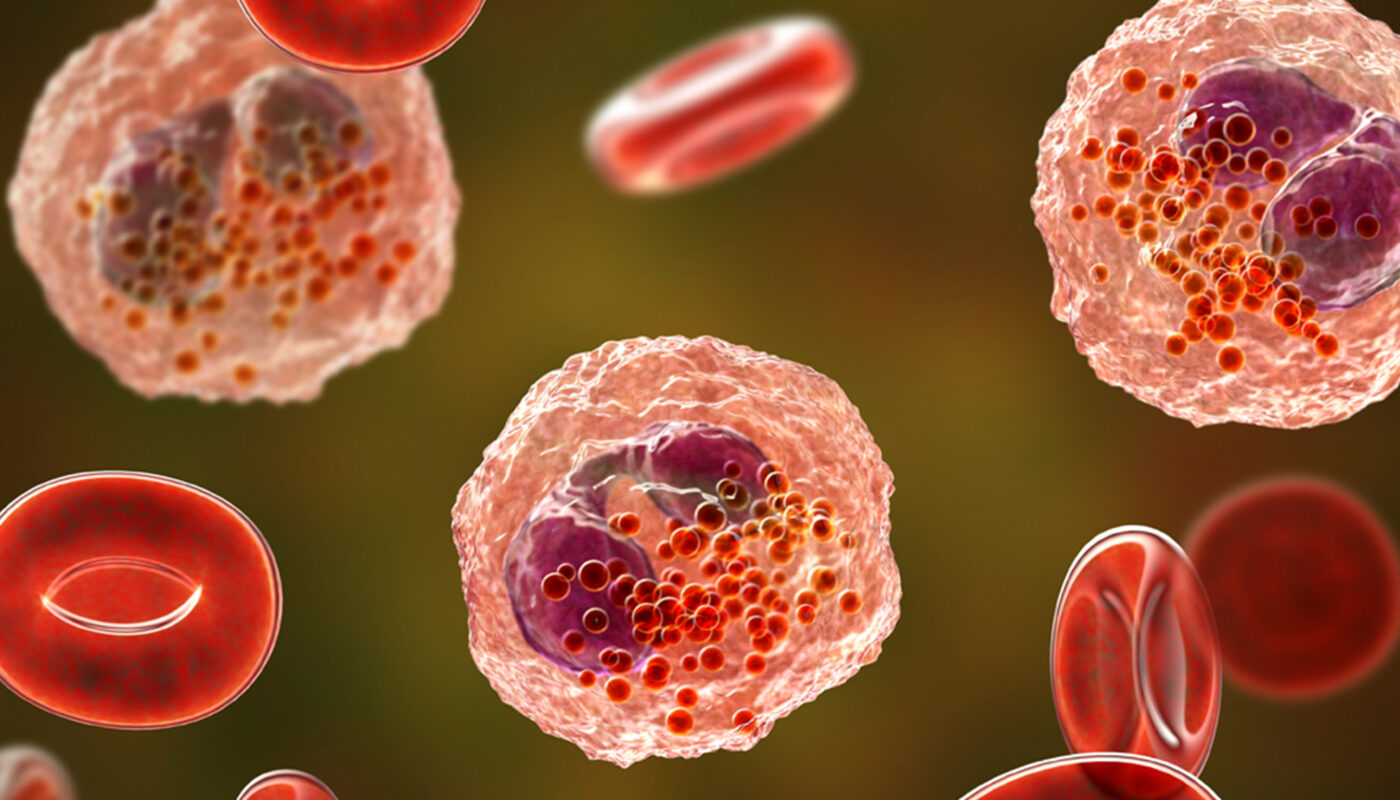
Pathogenesis
EoE is considered a primarily allergy-driven disease. This is supported by several observations:
– Treatment with topical steroids leads to histologic and symptomatic remission in the majority of patients, indicating an inflammatory and not structural basis to the disease.
– EoE patients have elevated levels of immunoglobulin E (IgE) and eosinophil-associated cytokines/chemokines in their esophageal tissues and blood.
– Food allergen avoidance based on test results leads to remission in many cases.
– An association with atopic disorders like asthma is observed.
– Eosinophils accumulate in the esophagus in response to specific food allergens.
The exact pathogenic mechanisms underlying EoE continue to be elucidated. Current hypotheses suggest that antigen exposure in a genetically susceptible host leads to an inappropriate T-helper 2 type immune response and eosinophil recruitment/activation in the esophagus. Loss of immune tolerance to food allergens appears key in EoE pathogenesis.
Clinical Presentation
The most common symptoms of EoE include dysphagia, food impaction, chest pain and heartburn. Dysphagia may affect both solids and liquids. Food impaction occurs in 20-30% cases and commonly requires endoscopic food removal. Other symptoms can be vomiting, abdominal pain, food refusal in children.
The symptoms typically worsen with time if untreated. Symptoms are often episodic and related to specific food triggers. Growth delay may occur in pediatric EoE patients due to vomiting or refusal to eat. Long-standing EoE can lead to esophageal remodeling changes like rings/strictures.
Diagnosis
EoE is diagnosed based on clinical symptoms and histological findings. Endoscopy is performed and multiple biopsies are taken from the esophagus, especially from the distal and proximal parts. Histological examination must reveal ≥15 eosinophils per high power field in one or more biopsies for EoE diagnosis.
Emphasis should be made on ruling out other causes of esophageal eosinophilia like GERD, vasculitis, drug hypersensitivity reactions. PPI tests can help differentiate EoE from PPI responsive esophageal eosinophilia. Diagnostic tests for atopy/food allergy may include prick skin tests, patch tests and atopy blood tests (IgE, eosinophil counts). Esophageal dilation and bougienage helps in cases with strictures.
Management
The main treatment approaches for EoE include dietary modifications, topical corticosteroids and anti-reflux medications. Dietary therapy involves elimination of specific food triggers based on allergy tests followed by gradual re-introduction to identify causative foods. Amino acid-based elemental formula is effective in several cases.
Topical corticosteroid therapy with fluticasone propionate or budesonide administered via nebulizer is highly effective in inducing symptom control and histologic remission. Long-term maintenance therapy may be needed. Addition of acid suppression drugs can be tried if EoE symptoms overlap with GERD.
Refractory EoE cases may require montelukast, immunosuppressants or allergen-specific immunotherapy. Endoscopic dilatation helps in cases with esophageal strictures. Multidisciplinary approach involving allergists, gastroenterologists and dietitians provide best outcomes. Prognosis is good with long-term medical management to prevent complications of chronic eosinophilic inflammation.
EoE is an emerging disease of the esophagus driven by an allergic inflammatory response. Early diagnosis based on symptoms and distinctive histology is important to prevent long-term complications. Dietary therapy targeting food triggers and topical corticosteroids form the mainstay of management. With increasing awareness and advancing research, EoE is now better understood though many aspects related to its pathogenesis, natural history and newer treatment strategies require further evaluation. Integrated allergy and gastroenterology care provides optimal control of this chronic eosinophilic disorder.
Note:
1. Source: Coherent Market Insights, Public sources, Desk research
2. We have leveraged AI tools to mine information and compile it